How to Get Paid for IV Sedation
Estela Vargas, CRDH, CEO Remote Sourcing
A common lament from dentists and surgeons:
Dear Remote Sourcing,
“I can’t work on this patient without IV sedation, but I‘m not being paid by insurance for this service. It’s not fair! What can I do?” Dr. Free Service
Dear Dr. Free Service,
For the codes D9239 and D9243, you must take the write-off and allow the contracted fees. The patient did not meet the "medical necessity" criteria. It is a covered benefit if the patient has a qualifying health/mental condition. I reviewed his chart. Skin cancer and cholesterol do not qualify for medical necessity.
We can help you with this issue for future claims, but a standard narrative will not get these claims paid. A large section of anesthesia codes is listed in the Current Dental Terminology. Please note that some codes that were available in the recent past are now deleted and, if used, will cause a denial of your claim. Choosing the correct code for the situation is the best start to getting your claim paid.
Next is to know that some insurance will reimburse for IV sedation when delivered with qualifying oral surgery procedures, but it will vary greatly from plan to plan. For instance, D9222, D9223, D9239, and D9243 may be reimbursed if two or more teeth are extracted on the same appointment date. Other plans may require eight teeth or more extracted at once before the plan will consider payment for IV sedation.
Getting Insurance Verification on patients before treatment will eliminate some misunderstandings. Sometimes a pre-authorization is required and received before treatment.
If payment is unavailable with the dental plan, medical insurance may cover IV sedation. Be aware that the patient’s medical condition must meet the plan's criteria making IV sedation necessary.
Medical benefits are always primary to any dental benefits. Many payers require billing to the patient’s medical plan before submitting the claim to the dental policy. Sometimes dental policy will state whether to bill the medical first.
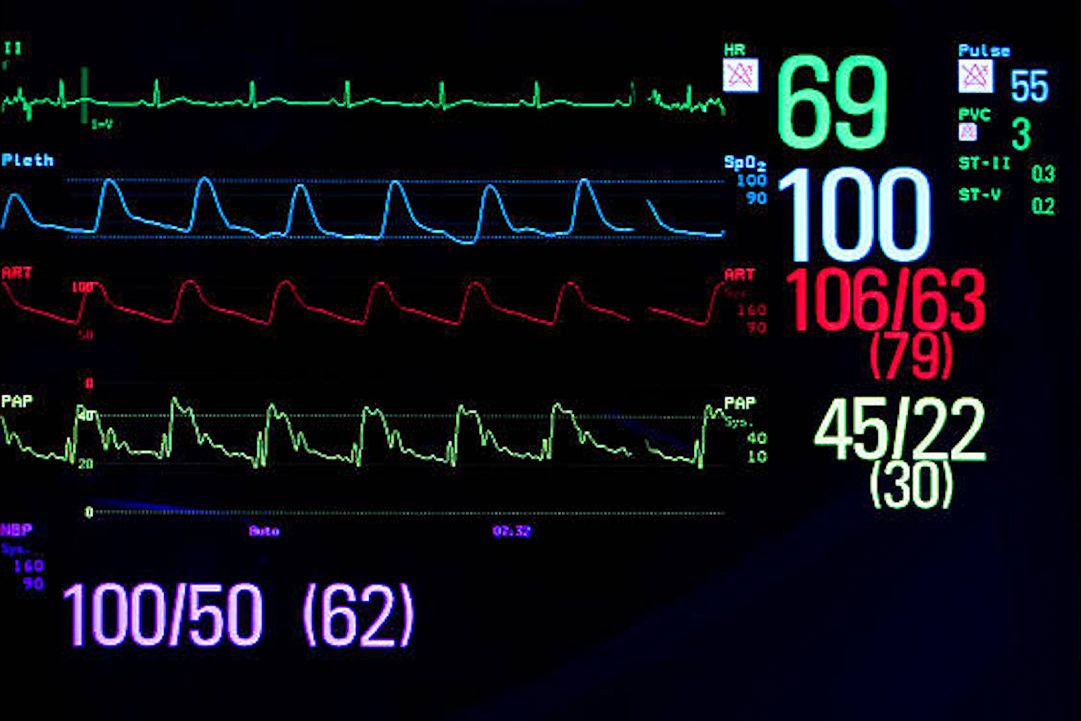
Most payers want documentation of the type of sedation and anesthesia permit number in the remarks section on the claim.
When dental and medical benefits are involved, you must provide a “medical necessity” statement to the patient’s chart/clinical notes and accompany the insurance claim. The statement explains the medical need for the patient to be sedated so that dental care can be delivered safely and considerate of the patient’s special needs. Some forms of medical necessity listed as acceptable as criteria for IV sedation are:
- Patient is allergic to local anesthetic.
- Patient has a medical condition such as asthma, epilepsy, severe autism, Down syndrome, Parkinsons, or Alzheimers.
- Patient needs the removal of bony impacted third molars.
- Patients under the age of 6 that require multiple extractions and restorations.
- Patient has a severe infection, and local anesthetic is unsuccessful.
Examples of winning appeals:
The following medical necessities were accepted to adjudicate the claims.
- The patient disclosed taking benzodiazepine in their medical history paperwork: Rationale: severe anxiety = auto-approval.
- The patient has spinal issues and cannot remain in the same position for an extended time: auto-approved appeal.
- The surgeon did an extraction, sinus lift, and immediate implant. I mentioned the Schneiderian membrane and the need for the patient to remain still to allow the surgeon to do their job without perforating the membrane for best results. It was approved on the first try.
Let Remote Sourcing take over your dental billing needs for less stress and peace of mind.